It’s the fifth day of National Breast Cancer Awareness Month 2022! Quick update from yesterday – my (hopefully) last breast reconstruction procedure went great! I’m home recuperating and enjoying love from my fur babies and my family. I haven’t looked at the result yet, but the left side of my surgical bra looks fuller. Hooray!
Now, back to the subject of breast cancer molecular subtypes! To recap, breast cancer isn’t a single disease. It is a collection of diseases that cause cells in the breast—specifically the cells that produce and deliver milk to nursing infants called epithelial cells—to grow uncontrollably, forming a tumor. Each breast cancer case is as unique as each person, but they can be classified based on similarities in how they look under a microscope (histology) and on the characteristics of their DNA (molecular).
Molecular breast cancer subtypes, which are crucial diagnostic tools used to determine the best and most appropriate course of treatment, include four subtypes recognized by scientists and clinicians based on their expression of hormone receptors (HR) for estrogen and progesterone (ER and PR) and their expression of the cell-surface receptor HER2: Luminal A, Luminal B, HER2-positive, and Triple Negative Breast Cancer TNBC.

Today’s post is all about the triple negative subtype, which do not express hormone receptors for estrogen and progesterone and also do not express express a cell surface protein receptor called HER2. That’s how it got its name, triple negative, because of the three receptors it does not express. These breast cancers have other ways of growing abnormally that don’t involve hormones or HER2, and they tend to grow very fast. For example, some TNBCs have higher higher than normal levels of EGFR receptors, which are in the same cell surface receptor family as HER2. Like HER2, EGFR normally tell breast cells to grow during normal development in puberty. In cancer, these receptors stay active and make breast cells grow when they shouldn’t, which is a key characteristic of breast cancer. Aside from targeting EGFR, a strategy being tested in clinical trials, people with TNBC have fewer treatment options with targeted therapies (therapies that inhibit hormone receptors and HER2) than other subtypes.
Aside from EGFR receptors, what make TNBC cells grow? There are several molecular pathways that become altered in TNBC. These pathways often function in normal breast epithelial cells telling them to grow when appropriate (cell surface receptors like EGFR, FGFR, and CSF1-R). When receptors on the surface of the cell becomes activated, they send signals to the breast cell that tells it to grow, like when your breasts are growing during puberty. Normally, after puberty, the receptor and related receptors are no longer activated and your breast cells stop growing. In breast cancer, your breast cells make too many receptors, which become constantly activated, making your breast cells grow abnormally, which is one hallmark of cancer. If other changes occur in your breast cells to form a cancerous growth, these receptors make the cancer cells grow uncontrollably.

One interesting characteristic of TNBC is that this subtype often has more interactions with the body’s immune system, meaning that immune cells travel to the tumor, get inside of it, and try to kill cancer cells and eliminate them from the body. Many cancer cells develop defenses against the immune system, using cell surface proteins like PD-1, PD-L1, and CTLA4 to shut down the immune cells. Tumors with lots of immune cells, called immunologically “hot,” may respond well to immune therapies that block the activity of PD-1, PD-L1, and CTLA4. The drug Pembrolizumab, which targets PD-1, is used to treat advanced TNBC. The drug Sacitiuzumab Govitecin was recently approved to treat TNBC. More on that below!
TNBC breast cancer is not as common as HR+ breast cancer, accounting for 15-20% of breast cancers. However, these breast cancers are often more aggressive and faster growing than HR+ breast cancer. They also disproportionately affect younger women and women of African descent. They are diagnosed by a pathologist based on analysis of gene and protein expression if ER, PR, and HER2 present in cancer cells in a biopsy and in the tumor after surgical removal. Low or no expression of these three receptors leads to a diagnosis of TNBC. This type of breast cancer, like most breast cancers, is first treated by surgery to remove the tumor.
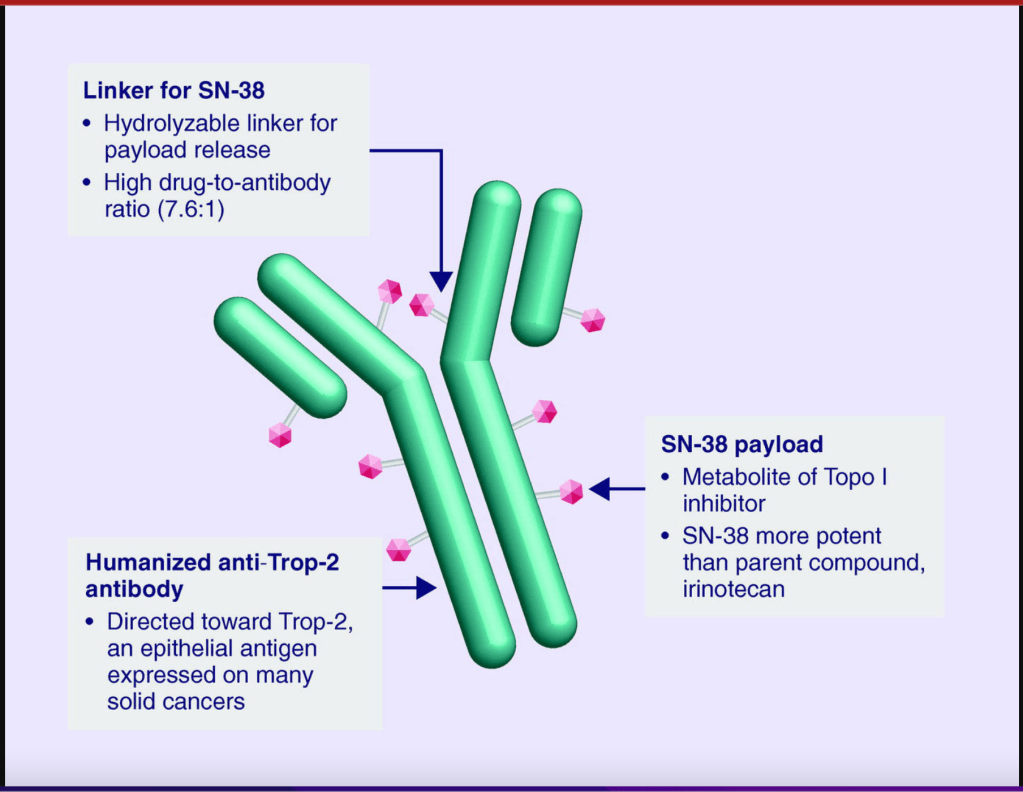
Follow-up treatments include chemotherapy, which was the only option for people diagnosed with TNBC for many decades. Recently, drugs developed specifically to treat TNBC have been approved and are being used in the clinic and undergoing additional testing in clinical trials to refine and optimize their ability to work with other drugs to kill more cancer cells. I discussed Pembrolizumab above. Let’s go over a little bit about Sacituzumab Govitecan. This drug binds to the cell surface protein Trop-2. Many TNBCs have higher than normal levels of Trop-2 on the surface of their cells. Sacituzumab Govitecan, approved in April of 2022, as a treatment for metastatic TNBC, is an antibody-drug conjugate that uses the an antibody against Trop-2 to carry a toxic drug directly to breast cancer cells with high levels ofTrop-2, targeting tumor cells and reducing damage to normal cells and tissues.
These treatments reduce the risk of the cancer from coming back, or recurring. They do come with some not-so-great side effects, which your oncologist should consider and help you with. Quality of life should always be a consideration when it comes to cancer treatment.
For more on TNBC, check out the American Cancer Association. As with other subtypes of breast cancer, early detection increases your chance of survival, so keep up with your routine mammograms and self-exams. Though TNBC is trickier to detect, screening mammography remains a vital tool for early detection of TNBC and other breast cancer cell types.

